Diabetes Mellitus occurs when the body either doesn’t produce enough insulin or can’t effectively use the insulin it produces.
Insulin is a hormone that plays a crucial role in regulating blood sugar levels. It allows cells to absorb glucose from the bloodstream to use as energy or store for future use. Insulin also helps lower blood sugar levels by promoting the storage of glucose in the liver and muscles.
There are several types of diabetes mellitus:
- Type 1 Diabetes: This occurs when the immune system attacks and destroys the insulin-producing beta cells in the pancreas, leading to little or no insulin production. It usually develops in children and young adults.
- Type 2 Diabetes: characterized by insulin resistance, where the body’s cells don’t respond properly to insulin. Initially, the pancreas produces extra insulin to compensate, but over time, it can’t keep up with the demand, leading to high blood sugar levels. Type 2 diabetes is more common in adults, especially those who are overweight or inactive.
- Gestational Diabetes: This type occurs during pregnancy when hormonal changes affect insulin sensitivity. It usually resolves after childbirth, but women who develop gestational diabetes are at a higher risk of developing type 2 diabetes later in life.
The common signs of diabetes mellitus include:
- Frequent urination: Excess sugar in the blood can lead to increased urination as the kidneys work to remove the excess glucose from the bloodstream.
- Increased thirst and hunger: Excessive urination can lead to dehydration, triggering increased thirst. Additionally, when cells are unable to receive adequate glucose for energy due to insulin resistance or deficiency, the body may signal increased hunger.
- Unexplained weight loss: Despite increased hunger and food intake, individuals with diabetes may experience unexplained weight loss due to the body’s inability to properly use glucose for energy. This can result in the breakdown of muscle and fat stores.
- Fatigue: When cells are unable to effectively utilize glucose for energy, it can lead to feelings of fatigue and weakness.
- Slow healing of wounds: Elevated blood sugar levels can impair circulation and weaken the immune system, leading to delayed wound healing.
- Tingling or numbness in the hands or feet: Over time, high blood sugar levels can damage nerves, a condition known as diabetic neuropathy, leading to tingling, numbness, or pain, often starting in the extremities.
factors causing Hypoglycemia:
- Exercising excessively: Intense or prolonged exercise can lead to #hypoglycemia if not balanced with adequate food intake or adjustments to insulin or medication doses.
- Delaying or skipping meals: Missing meals, especially after taking medication or insulin, can cause blood sugar levels to drop too low, leading to hypoglycemia.
- Misusing insulin: Using too much insulin or using it inappropriately can result in hypoglycemia, known as an insulin overdose.
- Extreme dietary practices: Completely eliminating carbohydrates from the diet can lead to hypoglycemia, as carbohydrates are the primary source of glucose for energy. It’s important to consume a balanced diet that includes complex carbohydrates in moderation.
- Excessive alcohol consumption: Alcohol can interfere with the liver’s ability to release glucose into the bloodstream, leading to hypoglycemia, even in individuals without diabetes.
- Combining medications without proper guidance: Mixing medications without consulting a healthcare provider can lead to interactions that affect blood sugar levels, potentially causing hypoglycemia or hyperglycemia.
Managing hypoglycemia involves consuming fast-acting carbohydrates to raise blood sugar quickly. This could include glucose tablets, fruit juice, soda, or candy. It’s also essential to monitor blood sugar levels regularly and adjust medication or lifestyle as needed.
To prevent hypoglycemia, you can:
- Always eat after taking your medications or insulin shot: Eating along with medication or insulin helps prevent hypoglycemia.
- Be careful not to over-exercise: While exercise is beneficial for managing blood sugar levels, excessive or intense physical activity can lead to hypoglycemia. Monitoring blood glucose levels before, during, and after exercise can help prevent this.
- Follow meal times carefully and avoid skipping meals: Consistency in meal timing helps regulate blood sugar levels by providing a steady source of glucose for energy. Skipping meals can cause blood sugar levels to drop too low.
- Eat a balanced diet, including carbohydrates, and practice #portioncontrol: Carbohydrates are an essential source of energy, but it’s crucial to consume them in moderation and pair them with protein, healthy fats, and fiber to prevent rapid spikes in blood sugar levels.
- Get diabetes medications prescribed by a doctor.
- Avoid combining medications without proper guidance: Mixing medications, including over-the-counter drugs and supplements, can affect blood sugar levels and interact with diabetes medications. Always consult with a healthcare provider before adding or changing any medications or supplements.
Hyperglycemia, or high blood sugar, can be caused by:
- Not taking enough insulin or diabetes medication: Insulin and other diabetes medications help regulate blood sugar levels. If doses are missed or not taken as prescribed, blood sugar levels can rise too high, leading to hyperglycemia.
- Eating too much food, especially carbohydrates: Carbohydrates have the most significant impact on blood sugar levels. Consuming large amounts of carbohydrates, especially refined sugars and starches, can cause blood sugar levels to spike. Monitoring portion sizes and choosing foods that are lower in carbohydrates can help manage blood sugar levels.
- Being inactive or not getting enough exercise: Physical activity helps your body use insulin more effectively, which can lower blood sugar levels. Being inactive or sedentary can lead to insulin resistance, making it harder to control blood sugar levels.
- Stress or illness: Stress and illness can cause hormones like cortisol and adrenaline to be released, which can raise blood sugar levels. Additionally, when you’re sick, your body may release more glucose into the bloodstream to fuel the immune response. Managing stress through relaxation techniques and taking care of yourself during illness can help prevent spikes in blood sugar levels.
Maintaining a normal blood sugar level involves:
- Monitoring blood sugar levels regularly: This helps you understand how your body responds to different foods, activities, medications, and stressors. It allows you to make informed decisions about your diet, exercise, and medication management.
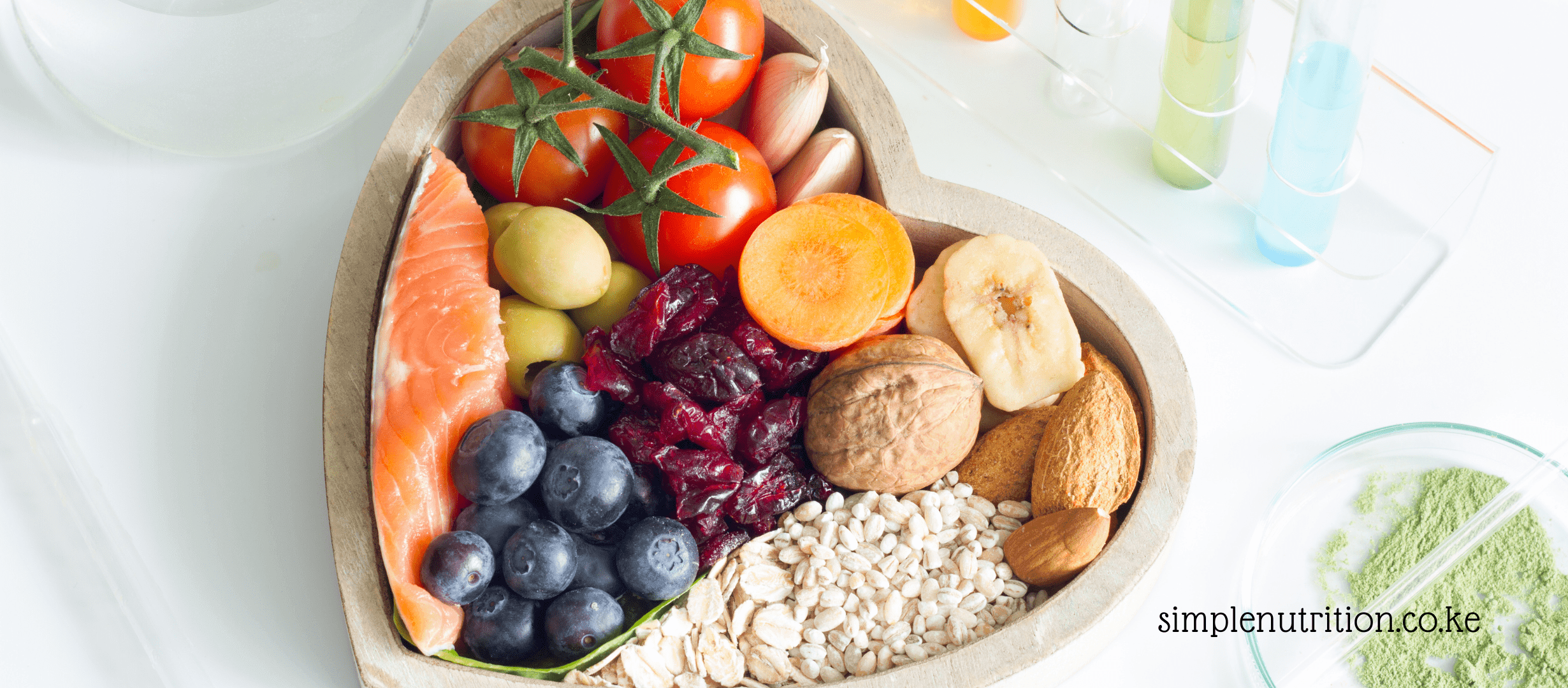
- Following a healthy diet that’s low in refined sugars and carbohydrates: A balanced diet rich in fruits, vegetables, lean proteins, and whole grains can help stabilize blood sugar levels. Avoiding foods high in refined sugars and carbohydrates can prevent spikes in blood sugar.
- Exercising regularly: Physical activity helps your body use insulin more efficiently, which can lower blood sugar levels. Aim for at least 30 minutes of moderate-intensity exercise most days of the week, but consult with your healthcare provider before starting any new exercise program.
- Taking medication as prescribed by a healthcare provider: If you’re prescribed insulin or other diabetes medications, taking them as directed is crucial for managing blood sugar levels effectively.
- Managing stress effectively: Stress can affect blood sugar levels by triggering the release of stress hormones like cortisol, which can raise blood sugar. Finding healthy ways to cope with stress, such as mindfulness, relaxation techniques, or hobbies, can help keep blood sugar levels stable.
- Maintaining a healthy weight: Being overweight or obese can increase insulin resistance and make it harder to control blood sugar levels. Losing weight through a combination of diet and exercise can improve insulin sensitivity and overall health. It’s essential to work with a healthcare provider to establish a realistic weight loss plan tailored to your individual needs.
Discover more from Simple Nutrition
Subscribe to get the latest posts sent to your email.